Coronavirus cases seem to rise when the variant is transmitted to the root.
Do you know anyone who got Covid now? You are not alone.
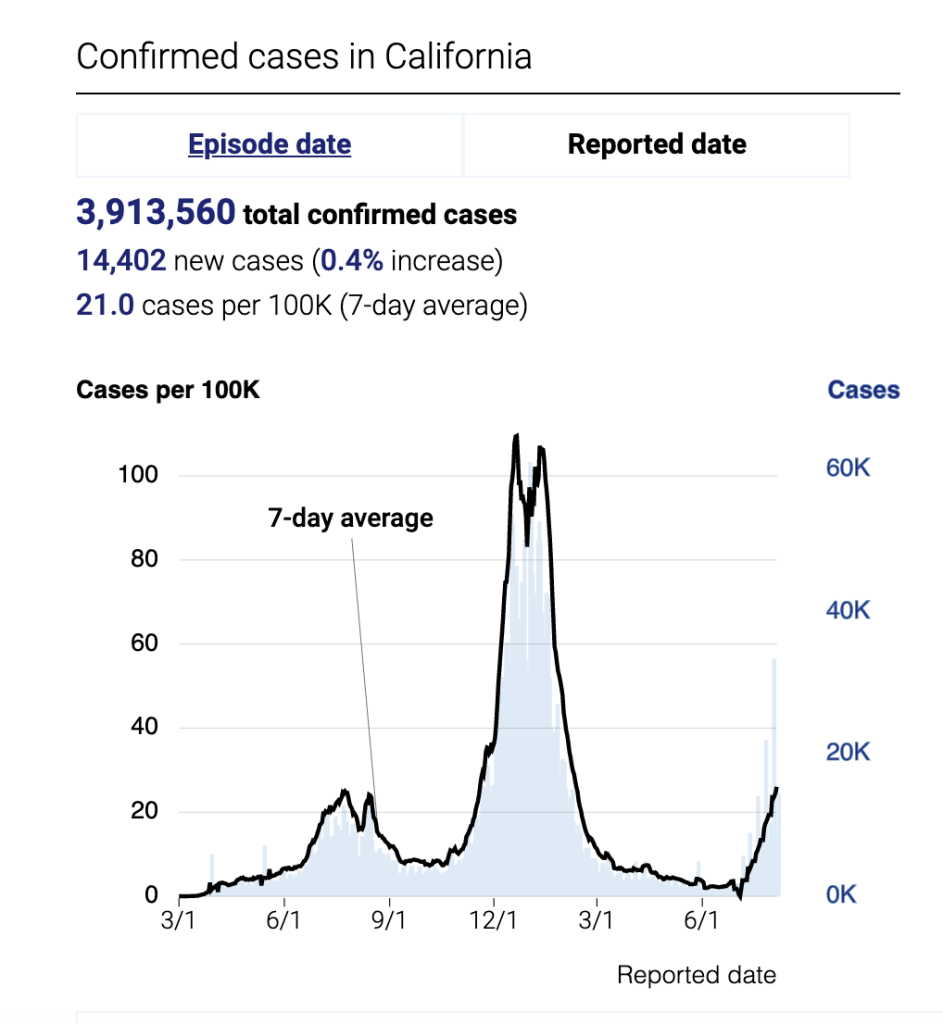
California is in the middle of the third-largest Covid surge, with around 19,000 new cases reported here every day, according to tracker The New York Times. The true number of people who are sick is definitely higher, because most tests on earth are not included in the official case count.
The good news: Most people who test positive do not become seriously ill. In fact, the number of people who die from Covid in California is now lower than almost anywhere in the pandemic. (This trend holds in many countries, as recently described by my colleague Benjamin Mueller.)
We can thank vaccines and boosters, immunity from Covid infection in advance and therapies such as Paxlovid – all seem to reduce the risk of severe disease.
Omicron subvariant BA.5 is fast becoming dominant in the United States. And it’s very good to infect people and bypass the immune system’s defenses, even if they’ve been vaccinated, encouraged and have got Covid, experts say.
“It’s very immune-evasive, and that’s why it causes problems,” said Dr. Eric Topol, professor of molecular medicine at Scripps Research in San Diego. “And came to California at the same time that basically we have this illusion that the pandemic is over.”
Topol told me that he knew many people who recently contracted Covid in San Diego, such as me in Los Angeles, where I live. C.D.C. consider the higher Covid risk in 38 of California’s 58 counties and recommend indoor masks in those places.
But unlike earlier in the pandemic, officials across California are reluctant to make a new ban. Alameda County reinstated the indoor mask mandate last month but canceled it three weeks from then.
Experts predict that without tighter rules or behavioral changes, the hyper-transmissibility of BA.5 will lead to a continued surge in cases in the coming weeks in California. There is also the possibility of a modest increase in hospitalizations and deaths, said Dr. Robert Kim-Farley, an infectious disease expert at the University of California, Los Angeles, Fielding School of Public Health.
“There’s a little bit of déjà vu that happens when we start to have other spikes,” he said to me. “I think we will continue to see a momentary increase, but I don’t expect we will see anywhere near the level of infection before the first Omicron wave.”
That’s because people who were exposed to previous Omicron strains, such as BA.1 and BA.2, seem to have protection from BA.5, although reinfection is possible. In other words, more Californians are vulnerable to Covid infections than when Omicron first appeared on the scene last year.
So, with all that in mind, how should we think about risk?
Dr. Bob Wachter, chairman of medicine at the University of California, San Francisco, explains it this way: It depends on what you’re trying to do.
If you are vaccinated, Covid does not have the same risk of death and hospitalization as you ever did. Stay up-to-date on your boosters to maintain that level of protection.
But even if you have all your shots, every Covid infection still opens the door to the possibility of developing a long Covid, a variety of symptoms that can be debilitating for some people.
Wachter recently recounted how a wife’s fatigue after a Covid infection increased her desire to avoid the virus. More than one in five adult Covid survivors in the United States can develop long -term Covid.
So, if you are trying to avoid infection at all, now is not the time in a public room indoors without a mask, such as in a restaurant, says Wachter.
In U.C. San Francisco, symptomatic Covid surgical patients swept for the virus as a precaution. About 6.5 percent of patients were testing positive, which indicates that about one in 16 people in the Bay Area who don’t seem very ill are infected with Covid, Wachter said.
The rest of the news
Academy Museum: The Academy Museum of Motion Pictures named Jacqueline Stewart, a film scholar who worked to make a long-delayed reality project, its new director and president.
Insurance commissioner race: Assemblyman Marc Levine claimed defeat in the state insurance commissioner race, reports The Los Angeles Times.
Hussle trial: A jury found Eric R. Holder Jr. guilty of first-degree murder for the murder of rapper Nipsey Hussle.
Drive reminder: The campaign that seeks to eliminate George Gascón, the Los Angeles County district attorney, gave more than 715,000 signatures Wednesday, but it’s not yet clear if the effort will be suitable, reports The Los Angeles Times.
Beach Access Mats: More beaches in Los Angeles are adding access mats on the sand for those who use wheelchairs and other assisted transportation, the Los Angeles Directory reports.
Pedestrian lanes: Los Angeles County’s public transportation agency is building bike and pedestrian lanes that will provide car-free mobility options between Inglewood and the east side of South Los Angeles, The LAist reports.
Boundary wall: The recently unveiled plan to replace the San Diego border fence at Friendship Park will block access to spaces used by people for years to meet loved ones separated by borders, KPBS reports.
Almonds: More than a billion pounds of unsold almonds are sitting in ports, waiting for supply chain problems to take over, reports The Los Angeles Times.
Delta drowning: The bodies of three people who went missing in the Sacramento-San Joaquin River Delta this weekend were recovered, The Sacramento Bee reports.
Wildfire: Favorable weather helped fight against a wildfire in the foothills of the Sierra Nevada mountains that has forced evacuations in two counties, The Associated Press reports.
Where we’re traveling
Today’s tip comes from Melissa Schilling, who lives in Santa Cruz. Melissa recommends state beaches on the Monterey Peninsula:
“In my opinion, the best place to walk, swim, surf, boogie board, tidepool, explore and enjoy the beach is Asilomar. Pacific Grove is good, clean and easy to find even in the peak tourist season.
Tell us about your favorite places to visit in California. Email your suggestions to CAtoday@nytimes.com. We will share more in a future edition of the newsletter.
And before you go, some good news
On a recent afternoon, Erin Alvarez beamed as she watched her daughters, Camila, 8, and Chloe, 4, try their hand at ceramics and craft wheels. They made stuff to bring to earth, and her mother got a photo to remember that time.
It’s the Sawdust Arts Festival, a nine -week event in Laguna Beach that typically draws more than 20,000 visitors. Guests can browse the works of dozens of local artists, or take art education classes.
This year’s festival, the 56th annual, begins on June 24 and will end August 28 Read more from The Daily Pilot.
Is it possible to have COVID-19 without a cough?

You can be infected with the coronavirus and not cough. If you have one, it may be mild and infrequent, or you may cough heavily at times. Remember that it is likely to have COVID-19 with minimal symptoms or no symptoms at all.
Is it possible to have COVID-19 if I only have a sore throat? Although rare, COVID -19 can only cause sore throat in around 5% -10% of cases. Throat pain associated with COVID-19 is relatively mild and lasts no more than 4–5 days.
When do symptoms of the coronavirus disease typically start?
People who got COVID-19 had a variety of reported symptoms-ranging from mild symptoms to severe symptoms. Symptoms can appear 2-14 days after exposure to the virus.
How long is the incubation period for COVID-19?
– Incubation period for COVID-19. Because the incubation period can be up to 14 days, the CDC recommends conducting screening tests at least once a week.
When do you start developing symptoms of the coronavirus disease?
Signs and symptoms of coronavirus disease 2019 (COVID-19) can appear two to 14 days after exposure. This time after exposure and before having symptoms is called the incubation period.
Can I have COVID-19 if I have fever?
If you have a fever, cough or other symptoms, you can get COVID-19.
What are some of the first symptoms of COVID-19?
Early symptoms reported by some people include fatigue, headache, sore throat or fever. Others experience a loss of smell or taste. COVID-19 can cause mild symptoms at first, but then become worse for five to seven days, with severe coughing and shortness of breath.
What temperature is considered a fever for COVID-19?
Fever is a common symptom of COVID-19. Body temperature of 100.4 degrees F or higher is generally seen in people who got COVID-19, although some people can feel such a fever despite normal temperature readings.
What do I do if I have mild symptoms of COVID-19?
If you have milder symptoms such as fever, shortness of breath, or cough: Stay on earth unless you need medical care. If you need to go in, first call your doctor or hospital for guidance. Tell your doctor about your illness.
What can I do to cope with the effects of COVID-19 quarantine?
Sedentary behaviors and low levels of physical activity can have a negative impact on an individual’s health, well -being and quality of life. Self -quarantine can also cause additional stress and mental health challenges to residents. Physical activity and relaxation techniques can be valuable tools to help you stay calm and then maintain your health during this time. WHO recommends 150 minutes of moderate intensity or 75 minutes of vigorous intensity physical activity per week, or a combination of both.
Can COVID-19 be transmitted through food?
Currently there is no evidence that people can catch COVID-19 from food. The virus that causes COVID-19 can be killed at the same temperature as other viruses and bacteria found in food.
What should I do after my last close contact with COVID-19?

Get tested at least 5 days after your last closing contact. Make sure your test result is negative and you remain without symptoms before leaving. If you have not been tested, avoid traveling until 10 full days after your last close contact with the person who got COVID-19.
What are some ways to deploy COVID-19? COVID-19 transmits when people breathe air that is contaminated with well droplets and small air particles. The risk of breathing is highest when people are close, but they can be inhaled at greater distances, especially indoors.
Can the coronavirus survive on surfaces?
It is not certain how long the virus that causes COVID-19 to survive on the surface, but it seems to behave like other coronaviruses. Recent reviews of the safety of human coronavirus on the surface find large variability, ranging from 2 hours to 9 days (11). virus.
How long can COVID-19 survive out in the air and on other surfaces?
Scientists found that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can be detected in aerosols for up to three hours, up to four hours in copper, up to 24 hours in cardboard and up to two to three days in plastic. stainless steel.
How long does the virus that causes COVID-19 last on surfaces?
New researchers evaluated the safety of COVID-19 virus on different surfaces and reported that the virus can remain viable for up to 72 hours in plastic and stainless steel, up to four hours in copper, and up to 24 hours in cardboard.
What are the organs most affected by COVID‐19?
The lungs are the organs most affected by COVIDâ € 19
How COVID-19 infect the body?
Viruses infect your body by entering healthy cells. There, the attacker makes a copy of himself and folds it throughout your body. The new coronavirus binds its spiky surface proteins to receptors in healthy cells, especially in your lungs.
What are the most common organs affected by COVID-19?
The lungs are the major organs affected by COVID-19; however, the virus can also affect other organs, such as the kidneys, brain, and liver. The lungs are the major organs affected by COVID-19.
Can COVID-19 be transmitted through food?
Currently there is no evidence that people can catch COVID-19 from food. The virus that causes COVID-19 can be killed at the same temperature as other viruses and bacteria found in food.
Can the coronavirus disease be transmitted through food or food packaging?
There is no evidence that human or animal food or food packaging is associated with the spread of the coronavirus that causes COVID-19.
Can I get COVID-19 from a food worker handling my food?
Currently, there is no evidence that food or meal packaging is associated with the spread of COVID-19.
What are the organs most affected by COVID‐19?
The lungs are the organs most affected by COVIDâ € 19
What organs are most commonly affected by COVID-19? The lungs are the major organs affected by COVID-19; however, the virus can also affect other organs, such as the kidneys, brain, and liver. The lungs are the major organs affected by COVID-19.
Can COVID-19 infect parts of the body other than the lungs?
Although it is known that the airways and upper lungs are the main sites of SARS-CoV-2 infection, there are indications that the virus can infect cells in other parts of the body, such as the digestive system, blood vessels, kidneys and, as follows. New study shows, firm.
What are the known coronaviruses that can infect people?
Human coronavirus can cause patients from the common cold to more severe diseases such as Middle Eastern respiratory syndrome (MERS, fatality rate ~ 34%). SARS-CoV-2 is the seventh coronavirus known to infect humans, after 229E, NL63, OC43, HKU1, MERS-CoV, and the original SARS-CoV.
What are the common side effects of COVID-19 vaccines?
The most commonly reported events with the COVID-19 vaccine are estimated side effects of the vaccine, such as headache, fatigue, muscle and joint pain, fever and chills and pain at the injection site. The occurrence of these adverse events is consistent with what is already known about vaccines from clinical trials.
How COVID-19 infect the body?
Viruses infect your body by entering healthy cells. There, the attacker makes a copy of himself and folds it throughout your body. The new coronavirus binds its spiky surface proteins to receptors in healthy cells, especially in your lungs.
How does COVID-19 enter the body?
We know that the virus primarily enters the body through the eyes, nose, or mouth and continues into the lungs, where the most severe infections occur. However, the virus replicates in cells, including the blood, and when it occurs, it changes the blood’s environment.
Is COVID-19 infectious after 7 days?
Most people who get COVID-19 are no longer contagious 5 days after they first have symptoms and have been fever-free for at least three days.
How long will I test positive after having COVID-19?
According to the Centers for Disease Control and Prevention, some people infected with COVID-19 can have the virus that can be detected for up to three months, but that doesn’t mean it’s contagious. When it comes to tests, PCR tests are more likely to continue the virus after infection.
Can you be contagious six days after your initial positive COVID-19 test?
Boston University researchers revealed that only 17% of people are likely to still be infected six days after the first positive test.
Are recovered persons with persistent positive test of COVID-19 infectious to others?
People who have tested consistently or tested positive for SARS-CoV-2 RNA, in some cases, the signs and symptoms of COVID-19 improved. While virus isolation in tissue culture has been attempted for such people in South Korea and the United States, live viruses have not been isolated. There is no evidence to date that people who recover clinically with persistent or recurrent viral RNA detection have transmitted SARS-CoV-2 to others. -CoV-2 RNA is no longer infectious. There is no strong evidence that antibodies that are developed to respond to SARS-CoV-2 infection are protective. If the antibody is protective, it is not known what antibody levels are needed to protect from re -infection.
How does the human body shed COVID-19?
Viruses make copies of themselves in human cells and then spread to other people. This is the process of spreading a virus. People who are sick with COVID-19 pass the virus from the nose and mouth. Although we cannot stop the spread of viruses, we can stop those viruses from infecting other people.
What is virus shedding with COVID-19? The spread of a virus is when a person removes a copy of the virus from their body. Patients with COVID-19 eliminate the virus around 14 days, starting 2 to 3 days before they first have symptoms. Wearing a mask, social distance, and being vaccinated is the best way to prevent the spread of COVID-19.
How long could the COVID-19 virus linger in your body?
But for most people who are infected, virus levels in the body peak between three and six days after the original infection, and the immune system clears the pathogen within 10 days. Viruses that are released after this period are generally not contagious.
How long does it take to develop immunity after a COVID-19 infection?
Although immune protection correlates are not fully understood, evidence suggests that the development of antibodies following infection likely confers some level of immunity from subsequent infection for at least 6 months.
Can you still get COVID-19 after recovering from it?
Immunity is complicated and, true, you can still be infected again with COVID-19. In fact, a new study found that adults who were not vaccinated were twice as likely to be re-infected with COVID-19 than those who were vaccinated after they recovered from their illness.
How long after COVID-19 exposure could you be contagious?
Evidence suggests that most COVID-19 spread occurs approximately when symptoms begin, generally within 1–2 days before and 2–3 days after symptoms begin. However, spread is still possible up to 10 days after infection.
How common is Paxlovid rebound?
Mayo Clinic researchers reported today in the journal Clinical Infectious Diseases that less than 1% of patients at high risk of severe COVID-19 who were treated with Paxlovid (nirmatrelvir and ritonavir) had a second attack of COVID-19.
Can you be infectious before starting to develop COVID-19 symptoms?
“People who got COVID-19 are considered infectious starting two days before they develop symptoms, or two days before the date of a positive test if they don’t have symptoms,” according to the CDC.
Is COVID-19 still contagious after 5 days?
The CDC recommends isolating for five days after you start testing positive, and stopping your quarantine as long as you don’t have a fever for 24 hours and your symptoms improve. The agency’s guidelines add that you should keep wearing the mask until the 10th day â € ”basically a precaution if you are still infected.
How long do I need to stay in isolation if I have symptoms of COVID-19 but my symptoms are better?
If you persist in fever or your symptoms do not improve after 5 days of isolation, you should wait to stop your isolation until you are fever-free for 24 hours without using any medication that reduces your fever and symptoms that have not improved.
How long will I test positive after having COVID-19?
According to the Centers for Disease Control and Prevention, some people infected with COVID-19 can have the virus that can be detected for up to three months, but that doesn’t mean it’s contagious. When it comes to tests, PCR tests are more likely to continue the virus after infection.