California’s summer is complicated by a dizzying array of Omicron subvariants that have emerged in recent months.
The most dominant nationwide is BA.5, which officials say is not only highly contagious but has also increased the risk of being infected with the coronavirus again – perhaps just weeks after a previous case.
According to federal estimates, BA.5 comprised 65% of the country’s coronavirus cases in the week-ending Saturday, a staggering increase from a month ago when it accounted for 17% of cases.
Under the effects of the sub-variant:
So what does the rest of summer look like? Here’s a breakdown of what we know:
What can we expect?

California is clearly continuing to see a surge of cases from the superinfectious family of Omicron subvariants, namely BA.5.
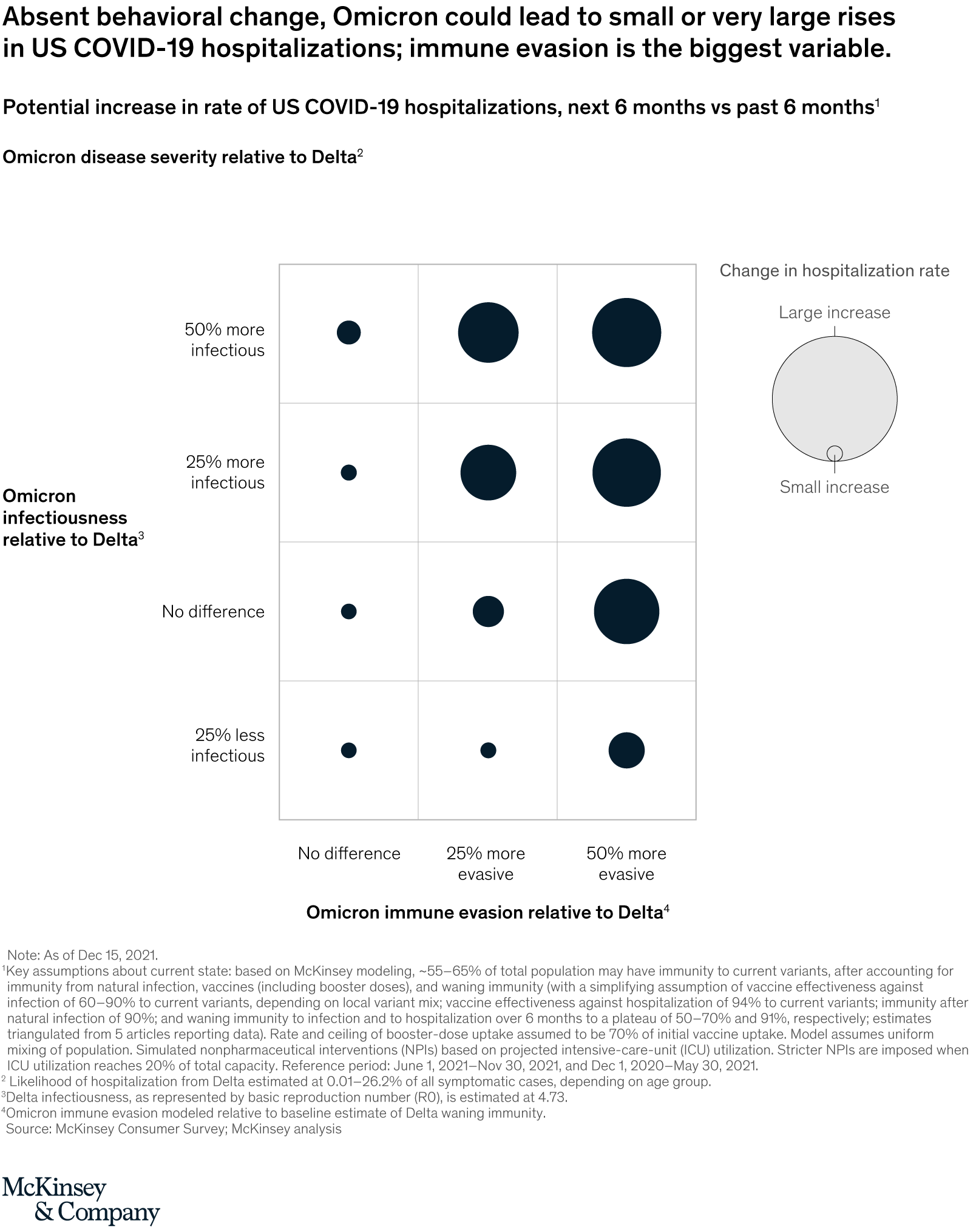
The number of coronavirus-positive hospital admissions is also rising, raising the possibility that facilities could come under renewed pressure. That’s not a certainty, however, as a fall or stabilization in infections would likely trigger the same thing in healthcare systems.
And while hospital admissions remain far lower than previous waves, the trend lines are worrying.
As of Tuesday, 4,377 coronavirus-positive patients were hospitalized statewide, including 1,170 in L.A. County. Over the past month, those numbers are up 61% and 97%, respectively.
In L.A. County, approximately 60% of coronavirus-positive patients in hospitals are being evaluated for reasons unrelated to COVID-19. But officials say they pose a potential burden on hospitals because additional resources are needed to prevent them from infecting others.
A forecast issued by the state suggests that coronavirus-positive hospital admissions will continue to increase over the next two weeks before declining. If the model is correct, the number of predicted hospital admissions at the peak “won’t compare to any previous increases that we’ve seen,” said California epidemiologist Dr. Erica Pan in a briefing to the California Medical Assn. on Tuesday.
A big question is whether BA.5 will remain the dominant variant for a while longer. That forecast could eventually stabilize the situation in California and eventually lead to a drop in cases, Dr. Peter Chin-Hong, infectious disease expert at UC San Francisco.
A possible turning point in this scenario is the emergence of another Omicron subvariant, BA.2.75, which is a cause for concern in India. Scientists say it may spread quickly and bypass immunity from vaccines and previous infections. It’s unclear if it could cause more serious illnesses than other Omicron variants.
In previous waves, dominant strains such as Delta and Alpha remained relatively long and were not quickly displaced by their successors, meaning that someone infected might enjoy a high level of protection for several months.
That time frame has shortened significantly since Omicron first burst onto the scene late last year. Only since April have three different sub-varieties – BA.2, BA.2.12.1 and now BA.5 – been considered the dominant variety nationwide. This rapid succession means that someone can become infected with an earlier release of Omicron and then be reinfected with a newer version a few weeks later.
“Many people who have recently been infected can probably get the virus again in three or four weeks, as opposed to the old days where they have a three-month window period,” when re-infection is less likely, Chin-Hong said.
What about a new L.A. mask mandate?
Although L.A. County hospitals are not overwhelmed by COVID-19 patients, Ferrer said reinstating a universal mask mandate in case hospitalizations continue to increase is prudent.
“Waiting until hospitals are overwhelmed is way too late to do much about slowing transmission,” Ferrer said. “Actually, the time to slow transmission is when you start to see signs that your hospitals are becoming more busy.”
Ferrer has said that if L.A. County transitions to the CDC-defined high COVID-19 community level and stays there for two consecutive weeks, public health officials will reinstate a universal mask requirement in indoor public places for those ages 2 and older. Such an order could come into effect as early as July 29.
Should that happen, L.A. would be the only California county with a mask mandate, though the state Department of Public Health still strongly recommends masking indoors.
Unlike transmission rates, which account for coronavirus cases and test positivity rates, COVID-19 community levels account for both cases and hospitalization rates.
While some have questioned the effectiveness of a renewed mask mandate, “there is broad consensus in the scientific community that wearing a quality mask in indoor public spaces is an important tool in controlling the spread of COVID-19,” said Dr. Ashish Jha, the White House COVID-19 response coordinator, said during a Tuesday briefing.
This, he said, “prevents you from getting infected and it prevents you from spreading it to others.”
What evidence is there of the effectiveness of mask mandates?
Ferrer pointed to some studies that suggest universal masking commands have been effective in reducing virus transmission.
A study published in February in the journal Health Affairs says that in more than 400 U.S. counties, between March and October 2020, those with mask mandates had 35% lower coronavirus case rates than those without.
Another study released in March by the U.S. Centers for Disease Control and Prevention found that Arkansas school districts with universal mask requirements had a 23% lower incidence of coronavirus cases from August through October 2021 than districts without a mask requirement.
Another report showed how consistent use of quality masks can reduce the risk of infection.
The report released by the CDC in February says that consistently using a quality face covering — like an N95 or KN95 respirator — in indoor public places was associated with an 83% lower chance of testing positive for the coronavirus than using it who was not wearing a mask.
N95, KN95 and KF94 masks are far more effective than loose-fitting surgical masks, while surgical masks are more effective than cloth masks.
Are poorer communities being affected by more severe illness?
Poorer people are more likely to cause serious illness and death with COVID-19, even if they have the same vaccination status. During the spring, unvaccinated residents in poor communities were 11 times more likely to be hospitalized with COVID-19 than unvaccinated people in affluent areas. During that time, about 35 out of 100,000 unvaccinated residents in affluent areas were hospitalized with coronavirus infection, while about 400 out of 100,000 unvaccinated people in poor areas were hospitalized.
Differences persisted even among vaccinated individuals by income status. Vaccinated people in poor areas were about 1½ times more likely to need hospitalization than the same cohort in affluent areas. About 27 out of 100,000 vaccinates in affluent areas were hospitalized with coronavirus infection, compared with 38 out of 100,000 vaccinates in poor areas.
That means poorer L.A. County residents — who make up a significant portion of the economy, including food production, hospitality and tourism — are once again bearing the brunt of this latest wave of COVID-19.
“Family resources with fewer resources are more likely to have greater exposure at work, live in cramped quarters, and have one or more chronic medical conditions,” Ferrer said, “than wealthier people. “This puts these individuals at greater risk of suffering the severe effects of COVID. … Vaccination alone is not enough to eradicate the troubling injustices.”
L.A. County has a tremendous concentration of poverty and overcrowded housing, making the impact of a pandemic wave especially intense in a county of more than 10 million people. Of all Southern California’s coastal counties, L.A. County has the highest poverty rate and lowest median household income.
Older people are still more likely to die, but some of those who die are young. Fourteen new deaths were reported on Tuesday, including one person aged between 30 and 40 and four people aged between 50 and 64. Four deaths were between the ages of 65 and 79 and five people who died were aged 80 or older.
How about personal behavior?

It is also likely that some who have avoided infection are no longer using certain protective measures, or are exposed to family members and friends who have relaxed their protective practices.
People “take more risks; they move they travel,” Chin-Hong said. Even in San Francisco, a number of people aren’t wearing masks in places where it used to be commonplace, meaning there’s less peer pressure to wear a mask in areas where it used to be commonplace, Chin-Hong said.
That’s why it’s so important that people get vaccinated and boosted when they’re eligible, said CDC Director Dr. Rochelle Walensky.
“There’s a lot we can do to try to prevent these ICU stays,” she said.
Jha also noted, “Getting vaccinated now will not prevent you from getting a variant-specific vaccine later this fall or winter.”
And for those aged 50 and over, “If you haven’t received a vaccination in 2022 … please go for another vaccination,” he said. Whether you’re entitled to a first booster or a second, ‘get one now. It could save your life.”
What are my rights if I have an accident at work?
If your employer caused your accident through negligence, you are entitled to compensation at work. That means it is unlawful to be fired, disciplined or treated differently because of your right to compensation after an accident at work.
What is the employer’s responsibility if an employee is injured? After an injury or illness occurs, your employer must: Provide you with a work injury claim form within one business day of reporting a work-related injury or illness. Return a completed copy of the claim form to you within one business day of receipt.
What an employee should do if there is a workplace accident?
Once an accident or injury occurs, business owners should follow these steps:
- Take workers to a safe place. Remove injured workers from an area if it is dangerous and ensure other workers keep their distance.
- Assess the situation. …
- Help the injured. …
- Gather information and preserve evidence.
What should an injured employee do first?
First and foremost, assess the need for medical assistance. In an emergency, call 911 immediately. In non-emergency situations, consult and coordinate care with pre-arranged medical facilities established with your workers’ compensation provider’s network of medical providers.
What is the recovery time for the coronavirus disease?
Early research suggested that it can take your body 2 weeks to get over a mild illness, or up to 6 weeks for severe or critical cases. Recent data shows that recovery varies for different people, depending on things like your age and overall health.
How long does it take to recover from COVID-19? Fortunately, people with mild to moderate symptoms usually recover within a few days or weeks.
How can I speed up the healing time of the COVID-19?
Some of the things you can do to speed up your healing are similar to treating the flu or a bad cold. Eat healthy food. When you feel like eating, you’re providing your body with the vitamins and nutrients it needs to stay healthy. Limit sugary or highly processed foods like cookies and sodas.
How long could you experience “Long COVID” health problems?
Most people who test positive for some variant of COVID-19 typically experience some symptoms for a few weeks. People with long COVID-19 symptoms may have health problems four or more weeks after they are first infected, according to the CDC.
What can you take to lessen the mild COVID-19 symptoms at home?
Use over-the-counter medications as needed. If you have a high fever, you can take a fever reducer, such as acetaminophen, to bring it down. If you have a sore body, sore throat, or cough, a pain reliever can help relieve the discomfort these symptoms can bring.
How long are you contagious after being sick with COVID-19?
Most people with COVID-19 are no longer contagious 5 days after the first onset of symptoms and have been free of fever for at least three days.
Is self-isolation recommended for those with COVID-19?
Self-isolation at home has been recommended for people diagnosed with COVID-19 and people who suspect they have contracted it. Health authorities have issued detailed instructions for proper self-isolation. Many governments have mandated or recommended self-quarantine for entire populations.
How long does the virus that causes COVID-19 last on surfaces?
Recent research has assessed the survival of the COVID-19 virus on various surfaces, reporting that the virus can remain viable for up to 72 hours on plastic and stainless steel, up to four hours on copper and up to 24 hours on cardboard.
Is it normal for COVID-19 symptoms to last more than 10 days?
People with post-COVID illness can experience a variety of symptoms that can last more than four weeks or even months after infection. Sometimes the symptoms can even go away or come back.
How long do body aches and muscle pains last from COVID-19?
Body or muscle pain can be an early symptom of COVID-19, often occurring right at the onset of the disease and lasting 2-3 days on average. Unfortunately, COVID-19 body aches can sometimes last much longer and are commonly reported in people with long-term COVID-19 or post-COVID-19 syndrome.
Can COVID-19 symptoms get worse as it goes along?
COVID-19 can produce mild symptoms at first, which then become more intense over five to seven days, with worsening coughing and shortness of breath.
How can I speed up the healing time of the COVID-19?
Some of the things you can do to speed up your healing are similar to treating the flu or a bad cold. Eat healthy food. When you feel like eating, you’re providing your body with the vitamins and nutrients it needs to stay healthy. Limit sugary or highly processed foods like cookies and sodas.
What can you take to relieve mild COVID-19 symptoms at home? Use over-the-counter medications as needed. If you have a high fever, you can take a fever reducer, such as acetaminophen, to bring it down. If you have a sore body, sore throat, or cough, a pain reliever can help relieve the discomfort these symptoms can bring.
How long could you experience “Long COVID” health problems?
Most people who test positive for some variant of COVID-19 typically experience some symptoms for a few weeks. People with long COVID-19 symptoms may have health problems four or more weeks after they are first infected, according to the CDC.
Are symptoms of long-term COVID-19 syndrome similar to chronic fatigue syndrome?
This condition has no known cause but can appear like long-range COVID-19 symptoms. Chronic Fatigue Syndrome can cause severe lightheadedness, fatigue, brain fog, or something called Post-Exertional Malaise (PEM). PEM can occur after your child engages in more physical or mental activity than they are used to.
What are the most common organs affected by COVID-19?
Lungs are the main organs affected by COVID-19; However, the virus can also affect other organs such as the kidneys, brain and liver. Lungs are the main organs affected by COVID-19.
What can I drink if I have COVID-19?
Water should be your first choice for drinking liquids. But you can also have other drinks that contain water, such as lemon juice (diluted with water and unsweetened), tea, and coffee. Do not consume too much caffeine and avoid sweetened fruit juices, syrups, fruit juice concentrates and all sugary drinks.
What are the long lasting fruits and vegetables I should buy for COVID-19 quarantine?
The WHO recommends consuming at least 400 g (i.e. 5 servings) of fruit and vegetables daily. Citrus fruits like oranges, clementines, and grapefruit are good options, as are bananas and apples, which can also be cut into smaller pieces and frozen for later consumption or adding to smoothies. Root vegetables like carrots, turnips and turnips do likewise as vegetables like cabbage, broccoli and cauliflower are relatively non-perishable. Garlic, ginger, and onions are also great options to keep at home, as they can be used to add flavor to a variety of dishes.
What are the guidelines for proper nutrition during the COVID-19 quarantine?
For optimal health, it’s also important to remember to eat a healthy diet and stay hydrated. The WHO recommends drinking water instead of sugar-sweetened drinks. Limit or avoid alcoholic beverages for adults and strictly avoid in adolescents, pregnant and lactating women, or for other health reasons. Eat lots of fruits and vegetables and limit your intake of salt, sugar and fat. Choose whole grains over refined foods. For more advice on healthy eating during self-quarantine, see the WHO Regional Office for Europe tips on food and nutrition during self-quarantine.
What is the Families First Coronavirus Response Act (FFCRA)?
On March 18, 2020, President Trump signed the Families First Coronavirus Response Act (FFCRA), which provided state unemployment insurance agencies with additional flexibility and administrative resources to respond to the COVID-19 pandemic. The CARES Act (Coronavirus Aid, Relief, and Economic Security Act) came into force on March 27th. It expands states’ ability to provide unemployment insurance to many workers affected by the COVID-19 pandemic, including workers who are not normally eligible for unemployment benefits. For more information, see the resources available below.
How much will I be paid if I take paid sick leave under the Families First Coronavirus Response Act (FFCRA)? If you are taking paid sick leave because you are unable to work or telecommute due to a vacation requirement because you are (1) subject to a federal, state, or local quarantine or isolation order related to COVID-19; (2) have been advised by a healthcare provider to self-quarantine due to concerns related to COVID-19; or (3) have symptoms of COVID-19 and are seeking a medical diagnosis, you will be paid the higher of the following for each applicable hour: • your regular wage rate, • the applicable federal minimum wage under the FLSA, or • the applicable state or local minimum wage. In these circumstances, you are entitled to a maximum of $511 per day or $5,110 cumulative over the entire paid sick leave period.
What if an employee refuses to come to work for fear of infection?
Your policies, which have been clearly communicated, should address this. Training your employees is a crucial part of your responsibility. Local and state regulations may apply to your duties and you should comply with them.
What are some tips to manage and cope with job stress during the COVID-19 pandemic?
• Communicate about stress at work with your colleagues, supervisors and co-workers while keeping your distance (at least 1.80 m). â—‹ Identify things that cause stress and look for solutions together. â—‹ Talk openly with employers, workers and unions about how the pandemic is affecting work. Expectations should be clearly communicated by everyone. â—‹ Ask how you can access mental health resources in your workplace. • Identify the things over which you have no control and do the best you can with the resources you have. • Increase your sense of control by developing a consistent daily routine whenever possible – ideally one that resembles your pre-pandemic schedule.
Who is at greatest risk of infection from COVID-19?
Currently, individuals at greatest risk of infection are individuals who have had prolonged, unprotected close contact (i.e., within 6 feet for 15 minutes or more) with a patient with confirmed SARS-CoV-2 infection, regardless of whether the patient has symptoms .
Can I take paid sick leave to care for any one who is subject to a quarantine or isolation order or in self-quarantine?
no You can take paid sick leave under the FFCRA to care for an immediate family member or someone who regularly lives in your household. You can also take paid sick leave under the FFCRA to care for someone if your relationship creates an expectation that you will care for the person in a quarantine or self-quarantine situation and that person for care during quarantine or self-quarantine dependent on you. However, you may not take paid sick leave under the FFCRA to care for someone with whom you have no relationship. You also cannot take paid sick leave under the FFCRA to care for someone who is not expecting or dependent on your care during their quarantine or self-quarantine due to COVID-19.
Who is a covered employer that must provide paid sick leave and expanded family and medical leave under the FFCRA?
Generally, if you have fewer than 500 employees, you are a covered employer who must provide paid sick leave and extended leave for family and medical reasons. See Question 2 for more information on the 500-employee limit. Certain employers with fewer than 50 employees may be exempt from the law’s requirements to provide certain paid sick days and extended family and sick leave. See Question 4 and Questions 58 and 59 below for more information on this small business exemption. Certain public employers are also covered by the Act and must provide paid sick leave and extended leave for family and medical reasons.
What does it mean to be unable to work, including telework for COVID-19 related reasons?
You are disabled if your employer has work for you and any of the COVID-19 qualifying grounds set out in the FFCRA prevent you from performing that work either under normal circumstances at your normal workplace or through teleworking. If you and your employer agree that you will work your normal number of hours but outside of your normally scheduled hours (e.g. early morning or late evening), you can work and walking is not required unless there is COVID -19 qualifying reasons prevent you from following this schedule.
Who is a covered employer that must provide paid sick leave and expanded family and medical leave under the FFCRA?
Generally, if you have fewer than 500 employees, you are a covered employer who must provide paid sick leave and extended leave for family and medical reasons. See Question 2 for more information on the 500-employee limit. Certain employers with fewer than 50 employees may be exempt from the law’s requirements to provide certain paid sick days and extended family and sick leave. See Question 4 and Questions 58 and 59 below for more information on this small business exemption. Certain public employers are also covered by the Act and must provide paid sick leave and extended leave for family and medical reasons.
How do I compute the number of hours of paid sick leave for my employee who has irregular hours?
Generally, under the FFCRA, you are required to provide an employee with paid sick leave equal to the number of hours the employee is expected to work on average over a two-week period, up to a maximum of 80 hours if the employee works irregularly so that it is not possible is to determine the hours he or she would normally work over a two-week period, you need to estimate the number of hours. The estimate must be based on the average number of hours your employee should work per calendar day (not workday) during the six-month period ending on the first day of paid sick leave. This average must include all scheduled hours, including hours actually worked and hours for which the worker has taken leave.
Can employees take paid leave concurrently with expanded family and medical leave?
Yes. After the first two working weeks (typically 10 working days) of extended family and medical leave under the EFMLEA, you may request that your employee take extended family leave and medical leave and existing leave at the same time for the same hours, which would be available under your policies the worker in this case. This would likely include personal leave or paid time off, but not sick leave or sick leave unless your employee (or an insured family member) is ill.

