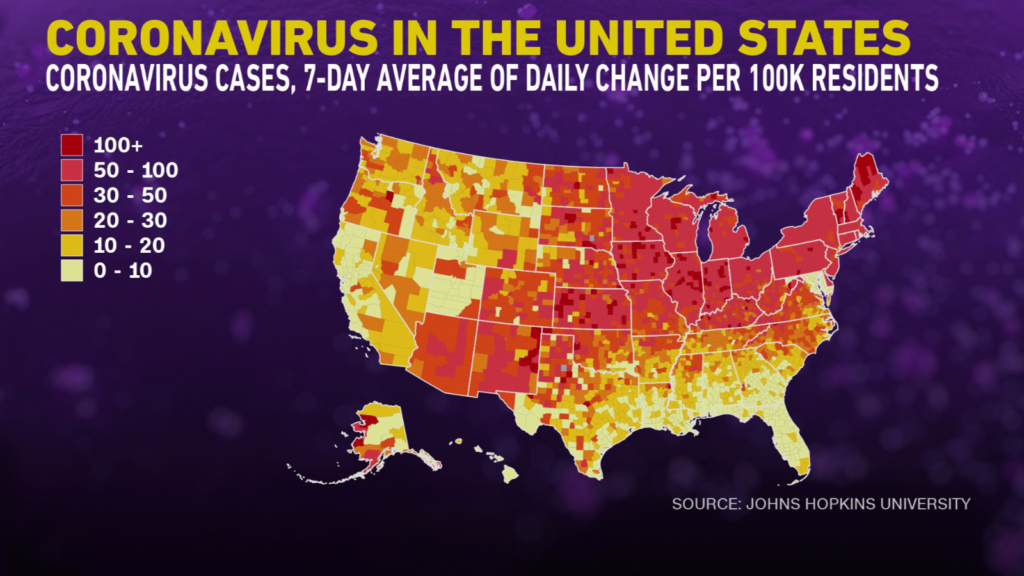
The number of coronavirus cases in California has deteriorated significantly over the past week, reaching levels not seen since the winter’s Omicron surge, raising concerns about the possibility of a large spike in infections this summer .
Weekly coronavirus cases have roughly doubled in much of California, including Riverside and Santa Barbara counties, as well as the Central Valley and Silicon Valley. They rose about 85% in Orange, San Bernardino and Ventura counties.
Statewide, the increase was 63%, bringing the case rate to 231 per 100,000 people. A rate of 100 and above is considered a high transfer rate.
Hospitalization rates, while rising over the past four weeks, remain low. Hospitals in two of California’s most populous regions, L.A. County and the San Francisco Bay Area, are not under pressure, and the rate of new weekly coronavirus-positive hospital admissions has remained at a fraction of the number in New York and other east coast cities.
California officials remain hopeful that a relatively robust effort to get residents to get booster shots, along with proposals to wear masks and get tested frequently, can help the state avoid the kind of sharp surge these people are seeing cities have experienced.
“The task before us is similar to the work we’ve had to do elsewhere for the past two and a half years: slowing transmission,” said Barbara Ferrer, L.A. County director of public health, in a statement. “We know what works – masking, testing and vaccination, and systems and policies that support the use of these and other effective safety measures.”
Nationwide, coronavirus cases are up more than 50% and hospital admissions are up more than 30% in the past two weeks, Dr. Peter Chin-Hong, an infectious disease expert at UC San Francisco.
The San Francisco Bay Area is currently home to the worst coronavirus case rate in California. The region is now being hit hard by new infections, likely because of the “latest transmissible variant,” whose contagiousness is approaching that of measles, one of the most easily communicable diseases for humans, Chin-Hong said in a briefing he gave to campus staff Friday .
Another factor in the rising case numbers may be that a relatively large number of people in the Bay Area have not been exposed to the coronavirus up to this point in the pandemic due to the region’s intense efforts to keep the virus in check.
dr Robert Kosnik, director of UC San Francisco’s occupational safety program, said at the briefing that he expects coronavirus cases to continue to rise for at least the next few weeks.
“I know this isn’t good news, but that’s what the data suggests,” he said.
The recent surge has been so disruptive that the Berkeley public school system has “only been able to fill about 50% of our teacher absences with substitute teachers,” the school district said in a statement. This has forced the administrators to help out in the classrooms.
Berkeley schools on Friday announced a new order to reinstate a mask mandate for students and staff for the remainder of the school year effective Monday, including indoor graduation ceremonies.
UC San Francisco is beginning to require universal masking at all large events with 100 or more attendees.
San Francisco had the highest case rate of any California county in the past week: 460 per 100,000 residents. The Bay Area reports a total of 369 cases per 100,000.
The Greater Sacramento area rate was 213; the San Joaquin Valley, 140; and rural Northern California, 139.
The overall rate for Southern California was 201, the rate for Los Angeles County was 224; San Diego County, 214; Ventura County, 201; Orange County, 171; Riverside County, 163; and San Bernardino County, 147.
Cases in Los Angeles County rose 16% week-over-week; San Diego County’s rose 33%.
Officials and experts in California can’t say for sure why the state’s rising coronavirus case numbers haven’t resulted in a greater number of hospital admissions, putting the state in a much better place than the East Coast.
One possibility is that California is simply behind the east coast, as it has been at earlier points in the pandemic.
But it’s also possible that a combination of booster shot rates among seniors and masking practices are at play, and that California could reasonably be hoping for a less severe spring and summer wave than New York.
About 67% of seniors in L.A. County and more than 80% of seniors in San Francisco have received a booster shot, compared to 58% of seniors in New York City.
Older people are at highest risk of dying from COVID-19. Among the seniors who have been vaccinated but are still dying from COVID-19, most have not received a booster shot, Chin-Hong said.
Wider mask use in parts of California, particularly among the elderly, could also quell the types of infections that can send people to the hospital.
L.A. County and the Bay Area have implemented local universal indoor mask orders for at least six months since last summer’s delta wave, while New York City declined to do so last summer and was under a statewide mask order for just two months during the fall and winter.
A longer duration of mask rules in L.A. County and the Bay Area may have prompted more people to continue wearing masks even after the state’s universal mask mandates ended.
Greater use of masks among vulnerable people can reduce the number of people who need to be hospitalized, and even if a masked person becomes infected, the mask can reduce the amount of virus entering the body and thereby the severity reduce the disease.
“And of course California has slightly better weather. But it’s still decent in New York now, so it’s not a big difference,” Chin-Hong said.
In L.A. County, the oldest residents have had one of the lowest coronavirus case rates to date, while younger adults and teens have the highest case rates. These trends could change; but that could explain why hospitals aren’t seeing any signs of on-site strains for now.
Even if California’s case count worsens dramatically, a later spring wave than New York may be beneficial as anti-COVID drugs like Paxlovid are now widely available — which weren’t the case earlier this year — and are health care providers and the public more conscious of getting them.
Paxlovid, a five-day pill regimen from Pfizer, must be taken within a few days of symptoms appearing. It reduces the risk of hospitalization or death from COVID-19 by 89% in higher-risk adults who are not hospitalized.
What is the case fatality ratio (CFR)?

Calculating the CFR Case Fatality Ratio (CFR) is the proportion of people diagnosed with a disease who die from that disease and is therefore a measure of severity among detected cases:
What does the mortality rate or death rate associated with the COVID-19 pandemic mean? The fatality rate is the number of people who have died from COVID-19 divided by the total number of people in the population. Because this is an ongoing outbreak, the death rate can change daily.
What percentage of Americans had COVID-19 as of April 2022?
April 26, 2022 — Nearly six in 10 Americans have already had COVID-19, an infection rate that increased dramatically from December through February, the CDC says.
What are the current statistics about long COVID?
Data for long COVID13.3% at 1 month or more post infection2.5% at 3 months or more based on self-reportMore than 30% at 6 months in hospitalized patients
What is the cumulative burden of COVID-19?
The cumulative burden of COVID-19 is an estimate of the number of people who may have been infected, sick, hospitalized, or died as a result of COVID-19 infection in the United States.
What is considered a COVID-19 case?
A COVID-19 case is an individual who has been determined to have COVID-19 based on a set of criteria known as the case definition. Cases can be classified as suspect, probable or confirmed.
What is a severe case of COVID-19?
According to the CDC, reported COVID-19 illnesses ranged from mild (in some cases with no reported symptoms) to severe illness requiring hospitalization, critical care and/or a ventilator. In some cases, COVID-19 diseases can lead to death.
What is the recovery time for the coronavirus disease?
Early research suggested that it can take your body 2 weeks to get over a mild illness, or up to 6 weeks for severe or critical cases. Recent data shows that recovery varies for different people, depending on things like your age and overall health.
What are the symptoms of the COVID-19?
Symptoms can appear 2 to 14 days after exposure to the virus. Common symptoms may include: fever or chills; Cough; Shortness of breath; Fatigue; muscle or body pain; Headache; new loss of taste or smell; Sore throat; congestion or runny nose; nausea or vomiting; Diarrhea.
What temperature kills the virus that causes COVID-19?
Research on the effects of temperature has shown that SARS-CoV-2, the virus that causes COVID-19, is sensitive to elevated temperatures, with over 99.99% inactivation in just a few minutes at 70°C (158°C). °F). However, this temperature is far beyond the limits of human comfort and could damage some building materials.
Can COVID-19 spread when swimming in water? Fact: Water or swimming does not transmit the COVID-19 virusSwimming does not transmit the COVID-19 virus through water. However, the virus spreads between people when someone is in close contact with an infected person. WHAT YOU CAN DO: Avoid crowds and maintain a distance of at least 1 meter from others, even when swimming or at swimming areas. Wear a mask when you’re not in the water and you can’t stay away. Clean your hands frequently, cover coughs or sneezes with a tissue or bend your elbows, and stay home if you feel unwell.
Can COVID-19 be transmitted through food?
There is currently no evidence that people can contract COVID-19 through food. The virus that causes COVID-19 can be killed at temperatures similar to other known viruses and bacteria found in food.
Can COVID-19 be transmitted through food or food packaging?
Because the number of virus particles that could theoretically be ingested by touching a surface would be very small and the amount required for infection by oral inhalation would be very high, the likelihood of infection from touching the surface of food packaging or from eating food is low is considered extremely low. The USDA and FDA are sharing this update based on the best available information from scientific panels around the world, including an ongoing international consensus that the risk of transmission of SARS-CoV-2 to humans via food and food packaging is extremely low.
Is the U.S. food supply safe?
There is currently no evidence that food or food packaging is associated with transmission of COVID-19. 19, is a virus that causes respiratory disease, not gastrointestinal disease, and foodborne exposure to this virus is not known to be a route of transmission by putting the virus on it and then touching your mouth, nose, or possibly your eyes, but it is not believed to be the main way of spreading the virus. It is always important to follow the 4 key food safety steps – clean, separate, cook and refrigerate.
How long does the virus that causes COVID-19 last on surfaces?
Recent research has assessed the survival of the COVID-19 virus on various surfaces, reporting that the virus can remain viable for up to 72 hours on plastic and stainless steel, up to four hours on copper and up to 24 hours on cardboard.
How long can COVID-19 stay on hard surfaces?
Scientists found that SARS-CoV-2, the virus that causes COVID-19, can be detected in aerosols for up to three hours and on plastic and stainless steel surfaces for up to three days. The results underscore the importance of hand washing and disinfecting commonly touched surfaces to protect against infection.
How long can the virus survive on surfaces?
It is not yet certain how long the corona virus will survive on surfaces. Preliminary studies suggest that the virus can persist for a few hours to several days.
In what conditions does COVID-19 survive the longest?
Coronaviruses die very quickly when exposed to UV light in sunlight. Like other enveloped viruses, SARS-CoV-2 survives longest when the temperature is at room temperature or below and when the relative humidity is low (
How long can COVID-19 stay airborne?
Transmission of COVID-19 by breathing airborne viruses can occur at distances of more than two meters. Particles from an infected person can travel throughout an entire room or interior. The particles can also linger in the air after a person leaves the room – they can stay in the air for hours in some cases.
How long can COVID-19 survive on surfaces?
Data from surface survival studies shows that under typical indoor environmental conditions, a 99% reduction in infectious SARS-CoV-2 and other coronaviruses can be expected within 3 days (72 hours) on common non-porous surfaces such as stainless steel, plastic and glass.
Where were first COVID-19 infections discovered?
The first known infections with SARS’ CoV’ 2 were discovered in Wuhan, China. The original source of virus transmission to humans remains unclear, as does whether the virus became pathogenic before or after the spillover event.
Where did the 2019 coronavirus disease outbreak begin? In 2019, a new coronavirus was identified as the cause of a disease outbreak that originated in China. The virus is now known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease it causes is known as coronavirus disease 2019 (COVID-19).
When was the first human coronavirus discovered?
Scientists first identified a human coronavirus in 1965. It caused a cold. Later that decade, researchers found a group of similar human and animal viruses and named them for their crown-like appearance. Seven coronaviruses can infect humans.
When was COVID-19 first reported?
This website provides information and guidance from WHO on the current outbreak of coronavirus disease (COVID-19), which was first reported from Wuhan, China on December 31, 2019.
Where was the first case of COVID-19 discovered?
Coronavirus disease 2019 (COVID-19) is defined as a disease caused by a novel coronavirus now called Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2; formerly known as 2019-nCoV) and first in an outbreak of respiratory disease cases in the city of Wuhan, Hubei province, China.
Where does the name COVID-19 come from?
The disease caused by SARS-CoV-2 was named COVID-19 by the WHO, the acronym deriving from “Coronavirus Disease 2019”. The name was chosen to avoid stigmatizing the origin of the virus in terms of populations, geography, or animal associations.
What does the word novel mean related to coronavirus?
The word Roman comes from the Latin word novus, meaning new. In medicine, “novel” usually refers to a strain of virus or bacteria that had not previously been identified. COVID-19 is an emerging disease caused by the novel or new coronavirus SARS-CoV-2, which has not previously been observed in humans.
What is the official name of the coronavirus?
From “Wuhan virus” to “2019 novel coronavirus” to “COVID-19 virus,” the name of the new coronavirus that first emerged in China has evolved into its now official designation: SARS-CoV-2 (severe acute respiratory syndrome). corona virus 2).
When was COVID-19 first reported in the US?
January 20, 2020 CDC confirms the first US laboratory-confirmed case of COVID-19 in the United States from samples collected January 18 in Washington state.
When was the Omicron variant of COVID-19 detected in the U.S.?
Variant B.1.1.529 (Omicron), first detected in November 2021, was responsible for a December 2021–January 2022 spike in US infections with SARS-CoV-2, the virus that causes COVID-19 (1). .
When was the first case of the coronavirus disease detected in the United States in 2020?
Community transmission of COVID-19 was first detected in the United States in February 2020. As of mid-March, all 50 states, the District of Columbia, New York City and four US territories had reported cases of COVID-19.
Can the coronavirus disease spread faster in an air-conditioned house?
Waleed Javaid, MD, associate professor of medicine (infectious diseases) at the Icahn School of Medicine at Mount Sinai in New York City, says it’s possible but not likely. If someone in the home infected with the virus coughs and sneezes and is careless, then tiny virus particles could be circulating in the air in respiratory droplets. Anything that moves air currents in the room can spread these droplets, whether it’s an air conditioner, a window-mounted air conditioner, a forced heating system, or even a fan, according to Dr. Javaid.
Does ventilation help prevent the spread of COVID-19? Good ventilation, along with other preventive measures like social distancing and wearing masks, can help prevent you from catching and spreading COVID-19.
Can COVID-19 spread through HVAC systems?
While air currents within a given space can help spread disease among people in that space, to date there is no conclusive evidence that viable viruses were transmitted through an HVAC system, resulting in transmission of disease to people in other spaces led, which are supplied by the same system.
How long can COVID-19 survive out in the air and on other surfaces?
The scientists found that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can be detected in aerosols for up to three hours, on copper for up to four hours, on cardboard for up to 24 hours and on plastic for up to two to three days was stainless steel.
Can COVID-19 spread through air conditioning?
We don’t know for sure if the COVID-19 virus spreads through air conditioning. But we do know that when it’s hot and humid, people are more likely to stay indoors with windows closed – giving the virus more opportunities to spread. The coronavirus spreads through droplets that an infected person emits through coughing or sneezing, and through smaller droplets, infectious virus particles that can remain airborne for several hours. Outdoors, air currents can disperse and dilute the virus, making transmission less likely. You’re more likely to breathe the virus indoors with the windows closed, whether you have the air conditioning on or not. If you must be indoors with someone outside of your household, increase airflow by keeping windows open as much as possible.
How long can COVID-19 survive out in the air and on other surfaces?
The scientists found that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can be detected in aerosols for up to three hours, on copper for up to four hours, on cardboard for up to 24 hours and on plastic for up to two to three days was stainless steel.
How long can COVID-19 live in the air?
Research shows that the virus can survive in the air for up to 3 hours. It can get into your lungs when someone who has it exhales and you breathe in that air. Experts are divided on how often the virus spreads through the air and how much it contributes to the pandemic.
How long does the coronavirus live on different materials?
Depending on the surface, the virus can survive on surfaces for a few hours or up to several days. The new corona virus seems to be able to survive the longest on plastic and stainless steel – possibly up to three days on these surfaces. It can also survive on cardboard for up to 24 hours.