The number of coronavirus cases reported in California is on the verge of crossing the 10 million mark, a milestone that may significantly underestimate the total, but still has a sense of inevitability.
Since the hypertransmissible Omicron variant hit the scene in early December, the virus has warmed its way into apparently every family and social circle. Residents who have escaped the infection for years have been rescued in the resulting tidal wave of cases, but for many, the severity of the disease has been reduced by vaccinations, the availability of therapies and other factors.
A myriad of high-profile individuals who have recently tested positive – including Vice President Kamala Harris, Gov. Gavin Newsom and even Drs. .
“It’s getting easier and easier and getting harder to escape the infection. But that does not mean we put ourselves in a kind of mindset: ‘You know, and hell with that. I’ll just do anything. what I really want to do, “said Dr. Peter Chin-Hong, a UC San Francisco Infectious Diseases expert, during an interview Friday.
It is understandable that some see the coronavirus as unavoidable, especially in connection with massive numbers of new infections.
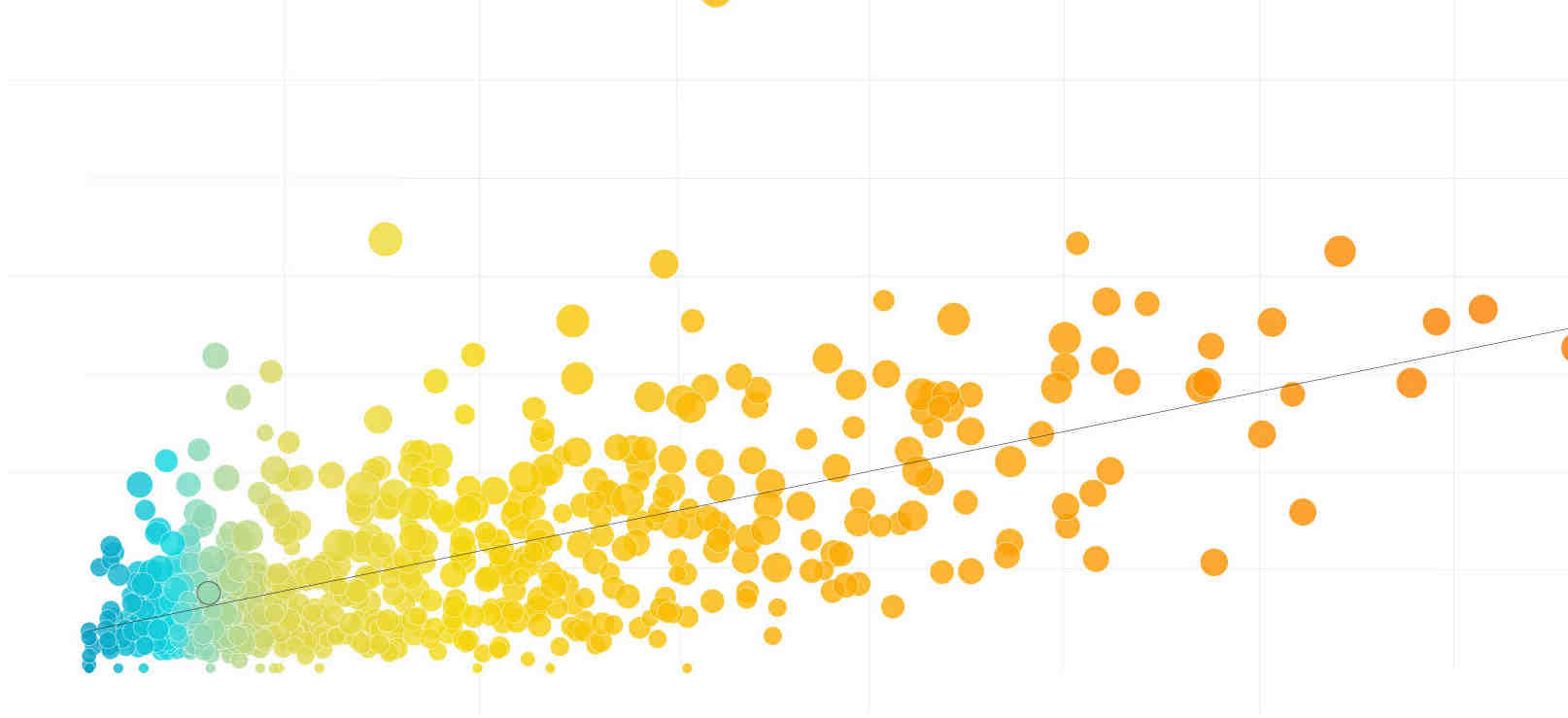
Nearly half of California’s officially reported cases – more than 4.9 million – have been counted since December 1, the day health officials confirmed Omicron’s presence in California, according to data compiled by The Times.
Officials note that these numbers are a sub-number, and possibly a significant one. According to data from the U.S. Centers for Disease Control and Prevention, the latest seroprevalence estimate for California – the total proportion of residents thought to have been infected with the coronavirus at some point – was 55.5% in February.
Nevertheless, that means there may be millions of Californians who have never contracted the virus.
Among them are Chin-Hong, as well as Dr. Robert Wachter, President of UC San Francisco’s Department of Medicine.
“The fact that I remain COVID-free in a fair number of people who remain cautious and fully vaccinated and bumped tells me that it is possible that we will continue to be so, so I do not buy the inevitability argument. ” Wachter said in an interview Friday. “On the other hand, there are a lot of people I know who have been just as careful as I have been in the last few months, so I think it’s some coincidence.”
Due to the proliferation of increasingly infectious Omicron subvariants, prevention of coronavirus has become an increasingly complicated proposition.
“It is possible because COVID-19 variants continue to evolve to become more transmissible and to gain the ability to avoid the protection of antibodies against infection, resulting in breakthrough infections in vaccinations and in those with previous disease, it will be difficult for many to avoid being exposed to COVID-19 beforehand, “said Dr. Robert Kim-Farley, an epidemiologist and infectious disease expert with the UCLA Fielding School of Public Health.
But infection is not inevitable, he added, and “everyone needs to be vigilant to avoid stress and prevent serious illness,” especially during periods of high community transmission.
“Masking when in full indoor settings and being vaccinated and strengthened is still the best protection. Even if one becomes infected and symptomatic, medications like Paxlovid will significantly reduce the severity of the disease, especially for people at higher risk. , “he told The Times in an email.
Although there are indications that the latest coronavirus wave in California may begin to level off, transmission remains increasing. During the week-long period, which ends on a Thursday, the state reported an average of 16,130 new cases per day – a decrease of almost 12% from two weeks ago, according to data compiled by The Times.
The new infections, however, have not created the same level of strain on hospitals everywhere as the previous current pandemic. However, the number of coronavirus-positive patients is constantly growing.
Since Friday, 3,169 such individuals have been hospitalized statewide – up 21% from two weeks ago. The number of patients treated in the intensive care units has also increased, to 331, but this number remains at the lowest of the whole pandemic.
It is true that not all patients are hospitalized for COVID-19 infections. The California Department of Public Health says about half are there “because of COVID-19 and not simply with COVID-19.” But officials say all coronavirus-positive individuals make demands on health facilities.
“Even though half of these patients cannot be hospitalized because they have COVID-19, they still affect hospital workload and exposure due to special infection control precautions and placement,” The Times said in a statement last week. .
But while this apparent script – less serious illness, even during a prolonged period of elevated transmission – is a promising development, officials and experts stress that it is impossible to predict the future course of COVID-19.
One area of concern is the proliferation of two Omicron sub-variants: BA.4 and BA.5. These are not only highly transmissible, but have shown the ability to re-infect survivors of former Omicron tribes.
In recent weeks, BA.4 and BA.5 have gradually accounted for a greater proportion of new coronavirus infections across the country. Over the seven-day period ending June 18, the CDC estimated BA.5 to account for 23.5% of new cases, and BA.4 to account for 11.4%.
As the growing footprint of the subvariants changes the way the pandemic in California remains to be seen. However, the World Health Organization recently noted that “the increase in the prevalence of BA.4 and BA.5 coincided with an increase in cases” in some regions, and in some countries this increase led to a current. Hospitalizations and ICU recordings. “
It is possible that the increase in hospitalizations is simply the numerical by-product of growing infections. As the WHO found, currently available evidence does not indicate any change in the disease severity associated with BA.4 or BA.5.
“It is still very early in our experience with BA.4 and BA.5, so we are reviewing the literature to see if there is data on it,” he said. Paul Simon, Chief Science Officer for the Los Angeles County Department of Public Health, said during a briefing Thursday. “And of course, if we see anything, even a slight increase in virulence for BA.4 and BA.5, that would raise a lot of concerns for us and, I think, increase the number of players to encourage the various safeguards. can take. “
Another case is the recent decision by federal health officials to authorize children as young as 6 months to receive either Pfizer-BioNTech or Moderna vaccination. While COVID-19 did not affect the youngest children as severely as other age groups, they were still vulnerable to infection – and could potentially spread the virus to others, increasing the risk of serious health problems.
“The fact that children under 5 are now being vaccinated, children aged 5 and over can get a booster, there is more Paxlovid around, all of which could keep the community viral load lower than it would be,” Chin-Hong said.
But at this time, the coronavirus is still widely circulating. In any infection not only carries the chance of short-term health effects with it, but the risk of developing “long covid” in which the symptoms can persist for months.
This is a possible outcome with which guard is all too familiar. His wife is still struggling with drowsiness and a few brain haemorrhages weeks after she became infected.
Some who develop long COVID, he said, will have prolonged symptoms that are “life-limiting in a way.” For others, those will “actually disable.” In any case, residents should not ignore the possibility.
Another symptom that recently infected people should be wary of is guilt – a feeling that the coronavirus is somehow proving that they have made a bad decision and are now paying the price.
“It is not a moral failure,” Chin-Hong said. “There are many reasons why it is so easy to get this particular infection, even if you take a measured approach to life.”
After all, people still have to go to work, make orders and take care of their children or other relatives when they get sick. And many are now taking the opportunity to rediscover activities that they were either unable or uncomfortable doing earlier in the pandemic.
“We are humans. We are social creatures. We were meant to go out and do things,” Wachter said. “All of us have to make choices about the level of risk we are willing to take. And that’s true when we get up in the morning and get out of bed; it’s true when we get on a plane; it’s true when we get in the car.”
That is not to say that precautions such as masks and overcrowded indoor settings and being vaccinated and strengthened, if justified, still do not make sense. But Californians do not need to beat themselves up if they take these steps and still catch the coronavirus.
“There are a lot of people who get infected who stay super careful,” Wachter said. “That’s the thing now, even very careful behavior is no guarantee you won’t get it. This damn thing is so incredibly contagious.
What are the guidelines for people who test positive for COVID-19?
Stay at home unless you need medical attention. Stay home from work and school, and avoid other public places, including the store. If you need to get out, avoid public transportation or ridesharing / taxis. Stay away (6 feet or more) from other people. Always wear a mask and wash or disinfect your hands frequently.
How long will most people continue to test positive for COVID-19? According to the New York Times, the omicron variant of the coronavirus moves rapidly, with viral levels usually less than five days after peaking after the virus is first detected. However, some people will continue to test positive for the virus even up to 14 days later.
Can you keep testing positive for COVID-19 and not be contagious?
According to the Centers for Disease Control and Prevention, some people who carry COVID-19 may have detectable viruses for up to three months, but that does not mean they are contagious.
Should I isolate and get tested if I have recovered from COVID-19 but I have symptoms again?
If a previously infected person experiences new symptoms consistently with COVID-19 3 months or more after the date of the previous disease onset (or date of the last positive viral diagnostic test [RT-PCR or antigen test] if the person has never experienced symptoms) , the person should do repeated viral diagnostic tests. However, serological tests should not be used to determine the presence or absence of SARS-COV-2 infection or re-infection. Those people who have a positive test result should be considered as infectious and remain isolated until they meet again criteria to stop isolation or transmission-based precautions. Contact tracing during the second episode of the person’s symptoms is justified.
How long are you contagious after being sick with COVID-19?
Most people with COVID-19 are no longer contagious 5 days after they first had symptoms and were fever-free for at least three days.
What should I do if I tested positive for COVID-19 or have symptoms?
If you experience COVID-like symptoms, you should isolate yourself from others for 5 full days after the onset of your symptoms, wear a well-fitting mask, be clinically evaluated for COVID-19, and be tested. Tell your healthcare provider if you are currently taking your COVID-19 vaccines.
Can people with mild COVID-19 symptoms recover at home?
People with mild symptoms who are otherwise healthy should manage their symptoms at home. On average, it takes 5 to 6 days from being infected with the virus until symptoms appear, but it can take up to 14 days.
How long should I stay in home isolation if I have a COVID-19 infection?
Positive. The test detects the virus and you have an infection. Stay home for at least 5 days and isolate yourself from others in your home. Tell your close contacts. Wear a well-fitting mask when you are around others. If available, an N95 or KN95 respirator is recommended. Pay attention to Symptoms.
How long are you contagious after being sick with COVID-19?
Most people with COVID-19 are no longer contagious 5 days after they first had symptoms and were fever-free for at least three days.
Is someone with COVID-19 still contagious after recovering?
The results, the team said, may indicate that a large number of people with COVID-19 are still likely to be contagious after the first five days of their illness, even if they feel fully recovered.
How long do I need to stay in isolation if I have symptoms of COVID-19 but my symptoms are better?
If you have further fever or your other symptoms do not improve after 5 days of isolation, you should wait to stop your isolation until you are free of fever for 24 hours without the use of fever-reduced medication and your other symptoms have improved.
Is it possible to get reinfected after recovering from COVID-19?
After recovery from COVID-19, most individuals have protection against recurrent infections. However, new infections occur after COVID-19. We are still learning more about these new infections.
How often can I get COVID-19? ‘A long-term pattern’ According to some infectious disease researchers, Covid-19 re-infections may become more common as time goes on and several variants continue to circulate – with some people potentially seeing third or fourth re-infections within a year.
Can you still test positive after recovering from COVID-19?
According to the Centers for Disease Control and Prevention, some people who contract COVID-19 may have detectable viruses for up to three months, but that does not mean they are contagious. When it comes to testing, however, PCR tests are more likely to continue to pick up the virus after infection.
How long could the COVID-19 virus linger in your body?
But for most infected people, virus levels in the body peak between three and six days after the original infection, and the immune system clears the pathogen within 10 days. The virus that disappears after this period is usually not infectious.
Is COVID-19 infectious after 7 days?
Most people with COVID-19 are no longer contagious 5 days after they first had symptoms and were fever-free for at least three days.
Can I get reinfected with COVID-19?
Studies suggest that new infections with SARS-CoV-2 with the same virus variant as the initial infection or new infections with a different variant are both possible; early new infection may occur within 90 days after initial infection.
How long does it take to develop immunity after a COVID-19 infection?
Even if the immune correlates of protection are not fully understood, evidence shows that antibody development after infection may give a certain degree of immunity to subsequent infection for at least 6 months.
Can you get COVID-19 if you already had it and have antibodies?
It is important to remember that some people with antibodies against SARS-CoV-2 may become infected after vaccination (vaccine breakthrough infection) or after recovering from a previous infection (newly infected).
How long does immunity last after COVID-19 infection?
Early on, researchers thought that natural immunity to COVID-19 lasted only about 2 to 3 months before disappearing. As the pandemic continued, experts began to find evidence that natural immunity could last almost a year after infection. But the variant Omicron came â € “and that changed everything.
Can you get COVID-19 if you already had it and have antibodies?
It is important to remember that some people with antibodies against SARS-CoV-2 may become infected after vaccination (vaccine breakthrough infection) or after recovering from a previous infection (newly infected).
What is the duration of natural immunity to COVID-19?
Natural immunity can decay within about 90 days. Immunity against COVID-19 vaccines has been shown to last longer. Both Pfizer and Moderna have reported strong vaccine protection for at least six months. Studies are underway to evaluate the full duration of protective immunity, including the Johnson & Johnson vaccination.
What is a COVID-19 rebound?
COVID-19 Rebound is when people with COVID-19 get better, then start getting symptoms 2-8 days after they recover. They can also test positive again. There have been reports of this happening with patients treated with Paxlovid.
What are the complications of COVID-19? Complications can include pneumonia, acute respiratory distress syndrome (ARDS), multi-organ failure, septic shock and death.
What are the organs most affected by COVID‐19?
The lungs are the organs most affected by COVIDâ € 19
What are the most common organs affected by COVID-19?
The lungs are the major organs affected by COVID-19; however, the virus can also affect other organs, such as the kidneys, brain, and liver. The lungs are the major organs affected by COVID-19.
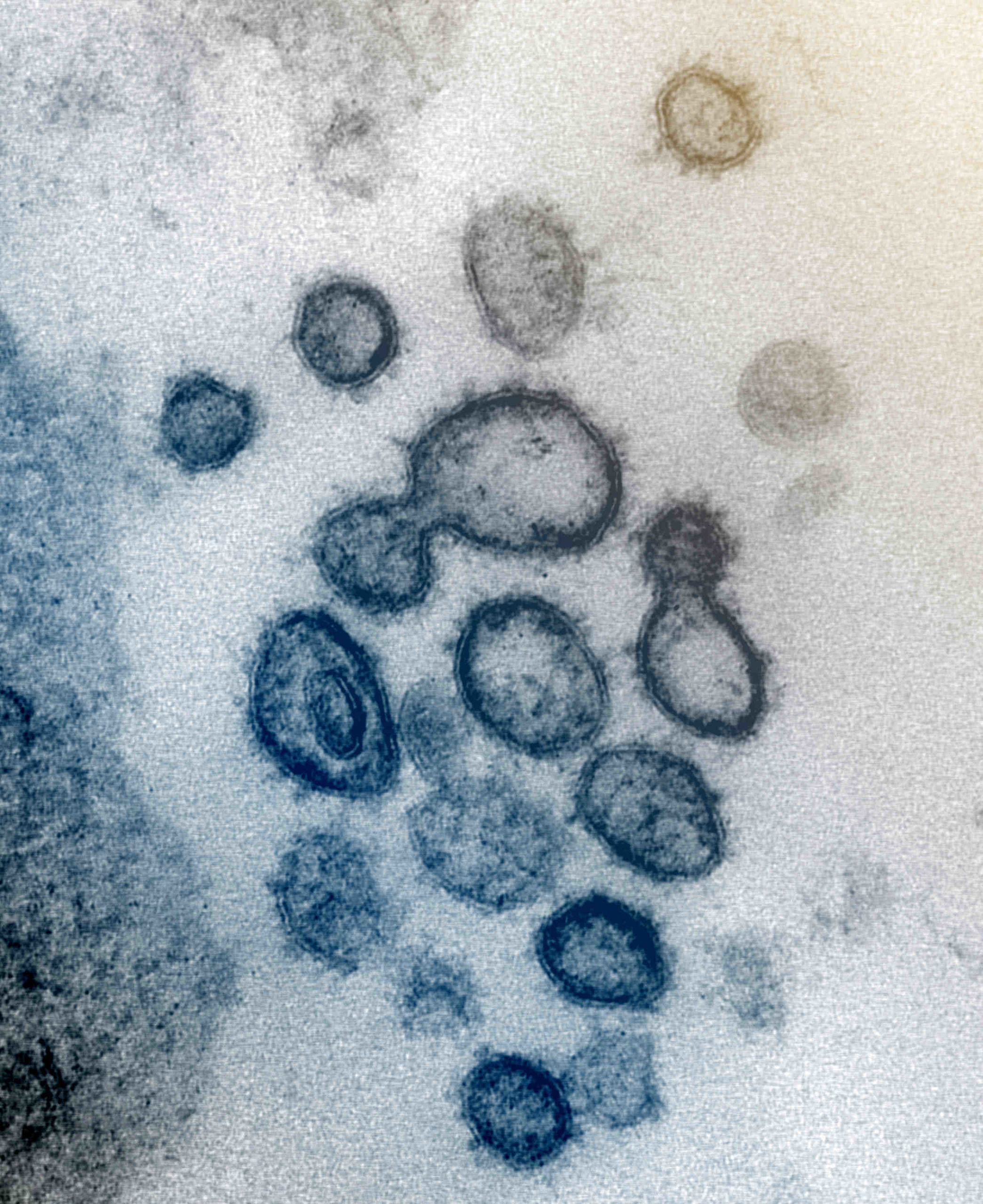
How COVID-19 infect the body?
A virus infects your body by entering healthy cells. There, the invader makes copies of itself and multiplies them throughout your body. The new coronavirus keeps its spiky surface proteins attached to receptors on healthy cells, especially those in your lungs.
How long does the virus that causes COVID-19 last on surfaces?
Recent research has evaluated the survival of the COVID-19 virus on various surfaces and reports that the virus can remain viable for up to 72 hours on plastic and stainless steel, up to four hours on copper, and up to 24 hours on cardboard.
Is it likely to catch COVID-19 from a surface?
It is unlikely to catch COVID-19 from a surface, but the risk still exists. Laboratory studies have found that the virus can last on different materials for varying amounts of time. We do not know if these findings are always valid in the real world, but we can use them as a guideline.
Can the coronavirus survive on surfaces?
It is not certain how long the virus that causes COVID-19 will survive on surfaces, but it may seem to behave like other coronaviruses. A recent study of the survival of human coronaviruses on surfaces found great variability, ranging from 2 hours to 9 days (11). of Virus.
Can people with mild COVID-19 symptoms recover at home?
People with mild symptoms who are otherwise healthy should manage their symptoms at home. On average, it takes 5 to 6 days from being infected with the virus until symptoms appear, but it can take up to 14 days.
How long should I stay in home isolation if I have a COVID-19 infection?
Positive. The test detects the virus and you have an infection. Stay home for at least 5 days and isolate yourself from others in your home. Tell your close contacts. Wear a well-fitting mask when you are around others. If available, an N95 or KN95 respirator is recommended. Pay attention to Symptoms.
What do I do if I have mild symptoms of COVID-19?
If you have milder symptoms such as fever, difficulty breathing or coughing: Stay home unless you need medical attention. If you need to go in, call your doctor or hospital first for guidance. Tell your doctor about your illness.
What are the rare but possible sexual side effects of COVID-19?

Scientists say that COVID-19 is known to damage blood vessels, and the virus seems to have damaged the vessels and penises of these patients and obstructed blood flow there, affecting sexual function.
Can COVID-19 affect the testicles? “A significant percentage of men experience testicular swelling or swelling of the epididymis after symptomatic COVID-19 infection,” says Drs. Deibert. A recent review of male reproductive health estimates that “10% to 22% of men with acute COVID-19 infection develop orchitis or epididymo-orchitis.
Can COVID-19 cause erectile dysfunction (ED)?
One study found that people infected with the virus were more than 5 times more likely to develop ED. In another small study, researchers took penile tissue samples from two men who were infected with COVID-19. One had severe symptoms, the other mild.
Can COVID-19 damage organs?
COVID-19 can cause permanent damage to various organs including the lungs, heart, kidneys, liver and brain. SARS CoV-2 first affects the lungs through the nasal passages. When the lungs are severely affected, it can affect the heart.
What are some of the neurological symptoms of COVID-19?
Neurological symptoms reported with acute COVID-19 include loss of taste and smell, headache, stroke, delirium, and encephalitis.
What are some of the symptoms of the COVID-19 Omicron strain?
Both coronavirus variants had common symptoms such as runny nose, headache and sneezing, but debilitating symptoms such as brain haze, dizziness and fever were less common in omicron cases.
Should I be worried about getting the COVID-19 Omicron variant?
While some have suggested that most people eventually get the coronavirus, you should do your best to avoid infection with Omicron – there is no reason to be deliberately infected so you have what you think will be a mild illness that will there is more. Immunity going forward, doctors say.
Is coughing a symptom of the Omicron COVID-19 variant?
Coughing and drowsiness are also more common symptoms for people taking Omicron.
How long do lingering symptoms last after COVID-19?
Symptoms. People with post-COVID conditions (or long COVID) may experience many symptoms. People with post-COVID conditions can have a wide range of symptoms that last for more than four weeks or even months after infection. Sometimes the symptoms may even disappear or come back.
How long could the COVID-19 virus linger in your body?
But for most infected people, virus levels in the body peak between three and six days after the original infection, and the immune system clears the pathogen within 10 days. The virus that disappears after this period is usually not infectious.
How long do body aches and muscle pains last from COVID-19?
Body pain or muscle aches can be an early symptom of COVID-19, often appearing at the onset of the disease and lasting an average of 2-3 days. Unfortunately, COVID-19 body pain can sometimes last much longer and is commonly reported in people with long COVID-19 or post COVID-19 syndrome.

