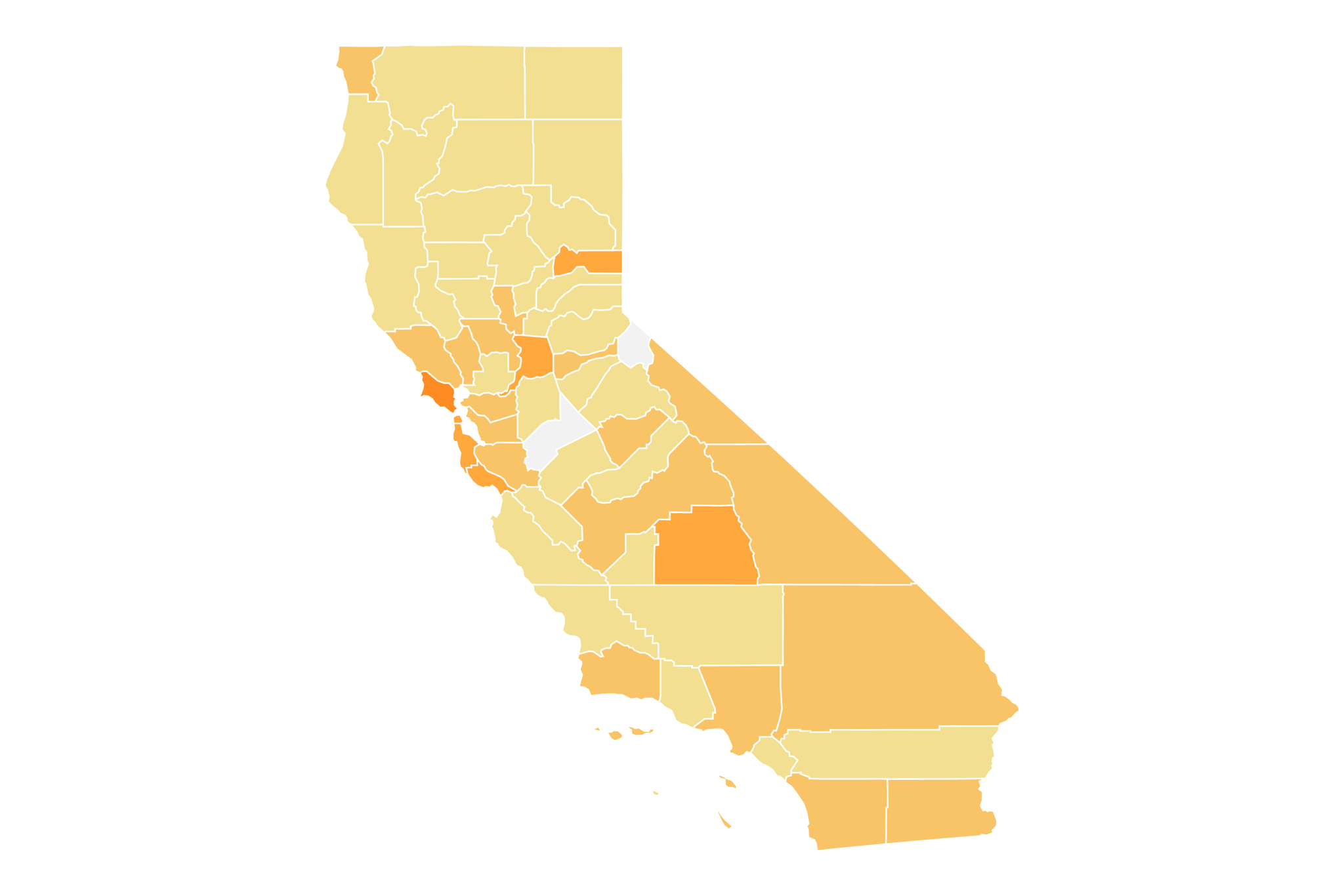
In a sign of how the new wave of coronavirus continues to spread across California, two-thirds of the state’s counties are now at the high COVID-19 community level where the U.S. Centers for Disease Control and Prevention has mandated universal masking in recommend indoor public spaces.
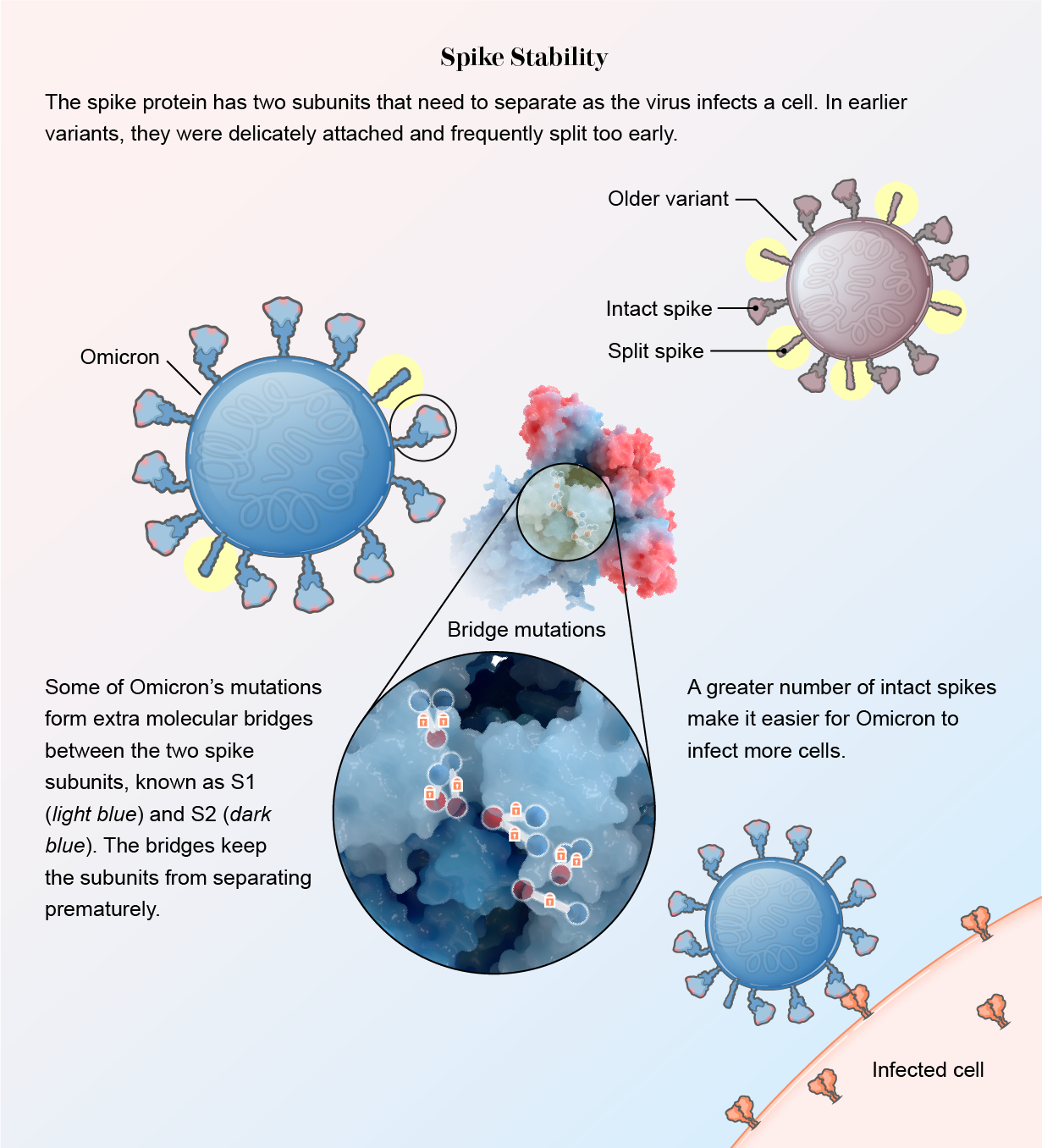
This comes as health officials warn of the coming weeks as two new ultra-contagious Omicron subvariants – BA.4 and BA.5 – spread. Experts believe the subvariants, which are not only particularly contagious but can also reinfect those who survived a previous Omicron infection, are a major factor in the ongoing transmission of the coronavirus across California.
So far, Los Angeles County health officials have not issued any new masking rules. However, they have warned that this could potentially be required later in July if new coronavirus-positive hospitalizations continue to rise. Though experts are concerned, there is still uncertainty about how serious a summer wave will get.
“With the continued increase in cases, and now that you’re seeing the corresponding increase in hospital admissions … we’re really concerned,” L.A. County public health director Barbara Ferrer said Thursday.
The California Department of Health and Human Services has strongly recommended universal mask-wearing in indoor public spaces since the state’s universal mask ordinance expired in February.
On Thursday, Kern, San Francisco, Ventura and San Mateo are the most populous counties in California that entered high COVID-19 community levels for the first time since the beginning of spring.
Ventura County on Thursday became the first Southern California county to enter the high COVID-19 community level since the first Omicron wave subsided.
Two-thirds of California counties are at the high COVID-19 community level.
(US Centers for Disease Control and Prevention)
COVID-19 community levels take into account coronavirus case and hospitalization rates.
Of California’s 58 counties, 38 are at the high COVID-19 community level. Approximately 16 million Californians live in these counties, which is 42% of the state’s population.
These include counties in the San Joaquin and Sacramento Valleys, the San Francisco Bay Area, and much of rural Northern California.
At the end of March and throughout April and May, not a single California county was at the high COVID-19 community level. But that changed in early June.
Los Angeles County has so far remained at the mid-level COVID-19 community level, where it has been since mid-May.
Health officials have announced they would reinstate a universal indoor public mask mandate for those ages 2 and older should L.A. County fall to high COVID-19 community levels for two consecutive weeks. L.A. County would maintain a universal mask mandate until it returns to mid-COVID-19 community level or lower for two consecutive weeks.
California’s coronavirus case rates have hit a stubborn plateau over the past month, reversing what appeared to be tempting signs in mid-June that cases were beginning to fall.
The data — as well as evidence that subvariants BA.4 and BA.5 dominate cases statewide — help explain why so many people across California appear to be reporting new infections. Officials say BA.4 and BA.5 appear to have the ability to reinfect people infected with previous Omicron strains.
As of Friday, Los Angeles County was averaging about 5,300 coronavirus cases per day, or 367 cases per week per 100,000 people, a 20% increase from the previous week. It’s the highest case rate in L.A. County since early February.
A rate of 100 or more cases per week per 100,000 population is considered high. Most counties in California have weekly case counts in excess of 200 — but case counts combined with hospitalization counts determine whether a county is classified under the CDC as having a high COVID-19 community level.
The San Francisco Bay Area still has California’s highest rate at 351 cases per week per 100,000 people. The Bay Area’s weekly case rate fluctuated between about 280 and 420 in June.
As of Friday, Southern California’s weekly case rate is 299; Greater Sacramento, 266; the Valley of San Joaquin, 255; and rural northern California, 200, according to the Times California coronavirus tracker.
California saw a 12% increase in coronavirus cases compared to mid-June, averaging more than 16,900 a day over the past week, according to data from The Times. Per capita, that is 303 cases per week per 100,000 inhabitants.
“Paxlovid is usually very well tolerated,” he says. Common side effects, which are usually mild, include: Altered or impaired sense of taste. Diarrhea.
Why is getting plenty of rest important for COVID-19 patients?
Expect to keep your body busy while battling a new virus. By giving yourself plenty of time to rest, you help your body provide the energy it needs to get the job done.
How can I speed up the healing time from COVID-19? Some of the things you can do to speed up your healing are similar to treating the flu or a bad cold. Eat healthy food. When you feel like eating, you’re providing your body with the vitamins and nutrients it needs to stay healthy. Limit sugary or highly processed foods like cookies and sodas.
Can COVID-19 symptoms get worse as it goes along?
COVID-19 can produce mild symptoms at first, which then become more intense over five to seven days, with worsening coughing and shortness of breath.
What are some signs of COVID-19 that need immediate medical attention?
• Difficulty breathing • Persistent pain or pressure in the chest • New confusion • Inability to wake up or stay awake • Pale, gray or blue skin, lips or nail beds, depending on skin tone
Is it normal for COVID-19 symptoms to last more than 10 days?
People with post-COVID illness can experience a variety of symptoms that can last more than four weeks or even months after infection. Sometimes the symptoms can even go away or come back.
What is the recovery time for the coronavirus disease?
Early research suggested that it can take your body 2 weeks to get over a mild illness, or up to 6 weeks for severe or critical cases. Recent data shows that recovery varies for different people, depending on things like your age and overall health.
How long does it take to recover from COVID-19?
Fortunately, people with mild to moderate symptoms usually recover within a few days or weeks.
How long does it take for symptoms to appear after exposure to COVID-19?
A wide range of symptoms have been reported in people with COVID-19, from mild symptoms to severe illness. Symptoms can appear 2-14 days after exposure to the virus.
How long can fatigue last after COVID-19 infection?
Fatigue typically lasts 2-3 weeks after COVID-19 infection, although some people may experience fatigue for 12 weeks or more after the infection has cleared.
How long do lingering symptoms last after COVID-19?
symptoms. Many symptoms can occur in people with post-COVID illnesses (or long-term COVID). People with post-COVID illness can experience a variety of symptoms that can last more than four weeks or even months after infection. Sometimes the symptoms can even go away or come back.
How do I cope with fatigue from COVID-19?
• Accept that fatigue is a real side effect of COVID-19. • Get a good night’s sleep. This can help your body conserve energy. Try relaxation techniques like mindful meditation, aromatherapy, yoga, and tai chi. These can help reduce stress and fatigue symptoms.
How long does it take to develop immunity after a COVID-19 infection?

Although the immune correlates of protection are not fully understood, evidence suggests that antibody development after infection likely confers some level of immunity against subsequent infection for at least 6 months.
How does your immune system behave after recovering from COVID-19? After you recover from a virus, your immune system retains a memory of it. This means proteins and immune cells in your body can recognize the virus and kill you if you become infected again, protecting you from the disease and reducing its severity.
Does your immune system get stronger after COVID-19?
Every time you contract a virus and recover from the disease, antibodies remain. These antibodies help your body fight off future infections, so you either don’t get sick or have milder symptoms.
How long could the COVID-19 virus linger in your body?
But in most infected people, virus levels in the body peak between three and six days after initial infection, and the immune system clears the pathogen within 10 days. Virus shed after this period is generally not contagious.
Can I get reinfected with COVID-19?
Studies suggest that reinfection with SARS-CoV-2 with the same virus variant as the initial infection or reinfection with a different variant is possible; early reinfection within 90 days of initial infection may occur.
How long does immunity last after COVID-19 infection?
Early on, researchers thought that natural immunity to COVID-19 lasted only about 2 to 3 months before waning. As the pandemic continued, experts found evidence that natural immunity could last almost a year after infection. But then the Omicron variant came along – and that changed everything.
How strong is immunity after a COVID-19 infection?
How strong is immunity after COVID-19 infection? According to the CDC, about 90% of people develop a set of protective antibodies after being infected with COVID-19. But how high these levels rise seems to be across the map.
What is the duration of natural immunity to COVID-19?
Natural immunity can wear off in about 90 days. Immunity to COVID-19 vaccines has been shown to last longer. Both Pfizer and Moderna reported strong vaccine protection for at least six months. Studies are ongoing to assess the full duration of protective immunity, including Johnson & Johnson’s vaccine.
How long does it take for antibodies to develop after exposure to COVID-19?
After an infection, it can take days to weeks for your body to produce antibodies.
Is it possible to develop immunity to COVID-19 after being exposed?
Additionally, there is hope that people who have been exposed to COVID-19 will also develop immunity to it. When you are immune, your body can recognize and fight the virus. It’s possible that people who have had COVID-19 will get sick again – and maybe infect other people.
How long do COVID-19 antibodies last?
It is not currently known how long antibodies persist after infection and whether the presence of antibodies confers protective immunity.
How long can you be infectious with COVID-19?
More than two years after the COVID-19 pandemic began, scientists are still unsure how long people who contract coronavirus remain contagious, reports The Wall Street Journal.
What is the difference between people with asymptomatic or pre-symptomatic COVID-19? Both terms refer to people who have no symptoms. The difference is that “asymptomatic” refers to people who are infected but never develop symptoms, while “presymptomatic” refers to infected people who have not yet developed symptoms but later develop symptoms.
How long does the virus that causes COVID-19 last on surfaces?
Recent research has assessed the survival of the COVID-19 virus on various surfaces, reporting that the virus can remain viable for up to 72 hours on plastic and stainless steel, up to four hours on copper and up to 24 hours on cardboard.
How long can COVID-19 survive out in the air and on other surfaces?
The scientists found that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can be detected in aerosols for up to three hours, on copper for up to four hours, on cardboard for up to 24 hours and on plastic for up to two to three days was stainless steel.
How long can COVID-19 survive on surfaces?
Data from surface survival studies shows that under typical indoor environmental conditions, a 99% reduction in infectious SARS-CoV-2 and other coronaviruses can be expected within 3 days (72 hours) on common non-porous surfaces such as stainless steel, plastic and glass.
Can asymptomatic people transmit COVID-19?
Yes, infected people can transmit the virus, both if they have symptoms and if they don’t have symptoms. Therefore, it is important that all infected people are identified through testing, isolated and given medical attention depending on the severity.
When should you stop isolation for COVID-19 if asymptomatic?
For people who test positive, are asymptomatic (never develop symptoms), and are not moderately or severely immunocompromised: Isolation can begin at least 5 days after the first positive virus test (Day 0 to Day 5, where Day 0 is the date of their sample) interrupted are collected for the positive test).
How long could you be contagious with COVID-19?
“You have to stay home for five days because you’re usually most contagious in the first five days,” said Dr. Allison Arwady, Commissioner of the Chicago Department of Health. “But these days between six and ten, some people can still spread viruses.”
What are the organs most affected by COVID‐19?
The lungs are the organs most affected by COVID 19
Can the COVID-19 virus affect your kidneys?
Does COVID-19 affect the kidneys? It can. In addition to attacking the lungs, the coronavirus that causes COVID-19 — officially known as SARS-CoV-2 — can also cause severe and permanent damage to other organs, including the heart and kidneys.
How COVID-19 infect the body?
A virus infects your body by entering healthy cells. There, the invader creates copies of itself and multiplies throughout the body. The new coronavirus connects its spiked surface proteins to receptors on healthy cells, particularly those in your lungs.
What is the Omicron variant of COVID-19?
Currently, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread worldwide as an omicron variant. This variant is a heavily mutated virus and is classified by the World Health Organization (WHO) as a variant of concern.

